Chronic Fatigue Syndrome (CFS), also known as Myalgic Encephalomyelitis (ME), is a complex and debilitating condition characterized by extreme fatigue that doesn’t improve with rest and worsens with physical or mental activity. For those living with CFS, finding effective treatment options can be life-changing. While there is no one-size-fits-all cure, a combination of therapies and lifestyle adjustments can help manage symptoms and improve quality of life. In this blog, we’ll explore the most effective treatment options for Chronic Fatigue Syndrome, backed by research and expert recommendations.
Understanding Chronic Fatigue Syndrome
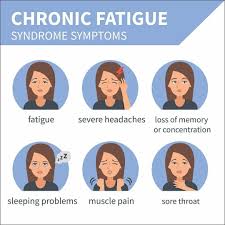
Before diving into treatment options, it’s essential to understand what CFS entails. The condition affects multiple systems in the body, including the immune, neurological, and endocrine systems. Common symptoms include:
- Severe fatigue lasting more than six months
- Post-exertional malaise (PEM), where symptoms worsen after physical or mental exertion
- Sleep disturbances, such as insomnia or unrefreshing sleep
- Cognitive difficulties, often referred to as “brain fog”
- Muscle and joint pain
- Headaches
- Sore throat and swollen lymph nodes
Because the exact cause of CFS remains unknown, treatment focuses on managing symptoms and improving daily functioning. Let’s explore the most effective strategies.
1. Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a widely recommended psychological treatment for CFS. It helps patients identify and change negative thought patterns and behaviors that may exacerbate symptoms. CBT is particularly effective for addressing the emotional and psychological toll of living with a chronic illness.
- How It Works: CBT focuses on breaking the cycle of fatigue by teaching patients coping mechanisms, stress management techniques, and ways to gradually increase activity levels without triggering post-exertional malaise.
- Evidence: Studies have shown that CBT can significantly reduce fatigue severity and improve overall functioning in CFS patients.
- What to Expect: A licensed therapist will work with you to set realistic goals, challenge unhelpful beliefs, and develop a personalized plan to manage symptoms.
2. Graded Exercise Therapy (GET)
Graded Exercise Therapy (GET) is a structured exercise program designed to gradually increase physical activity levels in CFS patients. The goal is to improve stamina and reduce fatigue without overexertion.
- How It Works: GET starts with low-intensity activities, such as gentle stretching or short walks, and slowly increases in intensity and duration over time. The program is tailored to the individual’s capabilities to avoid triggering PEM.
- Evidence: Research indicates that GET can improve physical function and reduce fatigue in some CFS patients. However, it’s crucial to work with a healthcare professional to avoid overexertion.
- What to Expect: A physical therapist will create a customized exercise plan and monitor your progress, making adjustments as needed.
3. Medications for Symptom Management
While no specific medication cures CFS, certain drugs can help manage symptoms and improve quality of life. Your healthcare provider may prescribe medications based on your specific needs.
- Pain Relievers: Over-the-counter pain relievers like ibuprofen or acetaminophen can help alleviate muscle and joint pain.
- Sleep Aids: For patients with sleep disturbances, medications like low-dose antidepressants or sleep aids may be prescribed.
- Antidepressants: Some CFS patients benefit from antidepressants, which can help with mood regulation, pain management, and sleep improvement.
- Antiviral Drugs: In cases where CFS is linked to viral infections, antiviral medications may be considered.
Always consult your doctor before starting any medication, as they can guide you on the best options for your condition.
4. Lifestyle Modifications
Making lifestyle changes is a cornerstone of managing CFS. Small adjustments to daily routines can have a significant impact on symptom severity and overall well-being.
- Pacing: Pacing involves balancing activity and rest to avoid overexertion. It’s essential to listen to your body and take breaks when needed.
- Sleep Hygiene: Establishing a consistent sleep routine, avoiding caffeine before bed, and creating a comfortable sleep environment can improve sleep quality.
- Stress Management: Techniques like meditation, deep breathing, and yoga can help reduce stress, which often exacerbates CFS symptoms.
- Dietary Changes: A balanced diet rich in whole foods, lean proteins, and healthy fats can support overall health. Some patients find relief by avoiding processed foods, sugar, and caffeine.
5. Alternative and Complementary Therapies
Many CFS patients turn to alternative and complementary therapies to supplement traditional treatments. While these approaches may not work for everyone, some individuals find them beneficial.
- Acupuncture: This ancient Chinese practice involves inserting thin needles into specific points on the body to promote healing and reduce pain.
- Massage Therapy: Regular massages can help alleviate muscle tension, improve circulation, and promote relaxation.
- Herbal Supplements: Some patients report symptom relief with supplements like magnesium, coenzyme Q10, and omega-3 fatty acids. However, always consult your doctor before trying any supplements.
- Mindfulness and Meditation: These practices can help reduce stress, improve mental clarity, and enhance emotional well-being.
6. Support Groups and Counseling
Living with CFS can be isolating, but connecting with others who understand your experience can provide emotional support and practical advice.
- Support Groups: Joining a CFS support group, either in person or online, allows you to share experiences, learn from others, and feel less alone.
- Counseling: Individual or group counseling can help you navigate the emotional challenges of living with a chronic illness and develop coping strategies.
7. Addressing Co-Existing Conditions
Many CFS patients have co-existing conditions, such as fibromyalgia, irritable bowel syndrome (IBS), or depression. Treating these conditions can improve overall health and reduce CFS symptoms.
- Fibromyalgia: Medications like pregabalin or duloxetine may be prescribed to manage pain and fatigue.
- IBS: Dietary changes, probiotics, and medications can help alleviate digestive symptoms.
- Depression: Antidepressants and therapy can address mood disorders that often accompany CFS.
8. Emerging Treatments and Research
Researchers are continually exploring new treatments for CFS, offering hope for future breakthroughs. Some promising areas of research include:
- Immunotherapy: This approach aims to modulate the immune system to reduce inflammation and improve symptoms.
- Stem Cell Therapy: Early studies suggest that stem cell therapy may help repair damaged tissues and improve energy levels.
- Microbiome Therapy: Research into the gut-brain connection has led to investigations into how probiotics and dietary changes can impact CFS symptoms.
While these treatments are still in the experimental stage, they represent exciting possibilities for the future of CFS management.
Tips for Working with Your Healthcare Team
Managing CFS requires a collaborative approach between you and your healthcare team. Here are some tips to make the most of your appointments:
- Keep a Symptom Diary: Track your symptoms, activity levels, and triggers to help your doctor identify patterns and tailor your treatment plan.
- Ask Questions: Don’t hesitate to ask your doctor about treatment options, potential side effects, and expected outcomes.
- Be Honest: Share your concerns, challenges, and goals openly with your healthcare provider.
- Seek a Second Opinion: If you feel your concerns aren’t being addressed, consider seeking a second opinion from a specialist familiar with CFS.
Final Thoughts
Chronic Fatigue Syndrome is a challenging condition, but with the right treatment plan, many patients can manage their symptoms and lead fulfilling lives. The key is to adopt a holistic approach that combines medical treatments, lifestyle changes, and emotional support. Remember, progress may be slow, but every small step counts.
If you or a loved one is struggling with CFS, don’t lose hope. Reach out to healthcare professionals, explore different treatment options, and connect with supportive communities. Together, we can navigate the complexities of CFS and work toward a brighter, healthier future.