In recent years, the healthcare industry has undergone a digital transformation, leveraging digital health technology to improve patient outcomes, streamline processes, and reduce costs. However, despite the rapid adoption of electronic health records (EHRs), health information systems, and various health technologies, one major obstacle continues to hinder the full potential of these advancements: interoperability.
Interoperability, in the context of healthcare, refers to the ability of different health systems and technologies to communicate, exchange, and use data seamlessly across various platforms. The integration of interoperability within healthcare systems is critical for improving patient care, enabling timely access to medical information, and ensuring a cohesive treatment approach across healthcare providers. However, achieving interoperability in healthcare is a complex process fraught with challenges. In this article, we will explore the importance of interoperability, the challenges it faces, and potential solutions to overcome these obstacles.
What is Healthcare Interoperability?
Healthcare interoperability is the capability of different healthcare information systems, devices, and applications to exchange, interpret, and use health-related data in a meaningful way. This means that whether a patient is receiving care from a primary care physician, a specialist, a hospital, or a telemedicine service, their health data should be able to flow across these different entities and be understood uniformly.
Effective interoperability allows healthcare providers to have access to a patient’s complete medical history, lab results, medications, allergies, and other critical health information, regardless of the system or technology used by different institutions. This leads to more informed decision-making, improved patient outcomes, reduced duplication of efforts, and better overall healthcare experiences.
The Importance of Interoperability in Healthcare Systems
- Enhanced Care Coordination
One of the key advantages of interoperability is the improvement of care coordination. When healthcare providers can seamlessly access and share patient data, they are better equipped to offer holistic care, reducing the risks of errors and misdiagnoses. For instance, if a patient is referred to a specialist or visits an emergency room, their medical history should be readily available, allowing for more informed decisions about their treatment plan.
- Improved Patient Outcomes
Interoperability enhances patient outcomes by ensuring that healthcare providers have accurate and up-to-date information at the point of care. When health data is exchanged and integrated smoothly, patients are less likely to undergo redundant tests, which saves time, money, and reduces patient discomfort. Additionally, clinicians are more likely to prescribe the right treatment, minimizing the chances of adverse events and improving overall treatment effectiveness.
- Increased Efficiency and Cost Savings
When data flows freely between healthcare systems, administrative tasks such as scheduling, billing, and medical recordkeeping become more efficient. Healthcare providers can avoid costly delays, reduce errors, and minimize duplicate tests or treatments. This leads to both operational cost savings and a more efficient healthcare system overall.
- Patient Empowerment and Satisfaction
Interoperability can also empower patients by giving them more control over their health information. Digital health technologies, such as health apps and patient portals, allow patients to access their medical records, test results, and treatment plans anytime, anywhere. This increased access can improve patient engagement, leading to better adherence to treatment regimens and more informed decision-making.
Challenges to Achieving Interoperability
Despite the clear benefits, integrating interoperability in healthcare systems faces several challenges. These challenges span technical, regulatory, and organizational domains, requiring multifaceted solutions.
1. Data Standardization Issues
One of the most significant barriers to interoperability is the lack of standardized formats for health data. Different healthcare providers and technology systems often use varying formats, structures, and terminologies to record and store data. For example, one hospital may store patient data in a proprietary format that is incompatible with another hospital’s system.
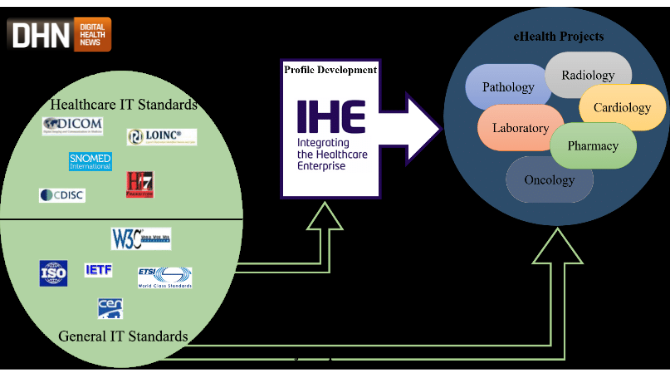
This lack of standardization makes it difficult for systems to communicate with one another, leading to inefficiencies and data discrepancies. Although there are some standards in place, such as HL7 (Health Level 7) and FHIR (Fast Healthcare Interoperability Resources), widespread adoption has been slow, and inconsistencies remain.
2. Data Privacy and Security Concerns
Given the sensitive nature of healthcare data, maintaining privacy and security is paramount. Many organizations are hesitant to share patient data due to concerns over data breaches and compliance with privacy regulations such as HIPAA (Health Insurance Portability and Accountability Act) in the United States.
Ensuring that data is shared securely while maintaining patient confidentiality can complicate the implementation of interoperability. Healthcare organizations must invest in robust security protocols to protect patient data and ensure compliance with privacy laws, making the integration of interoperability more complex and expensive.
3. Fragmented Healthcare Systems
Healthcare systems are often fragmented, with multiple stakeholders such as hospitals, physician practices, pharmacies, insurance companies, and laboratories using different technologies. Many of these organizations are slow to adopt new technologies, and some may have legacy systems that are incompatible with newer solutions.
This fragmentation makes it challenging to create a unified network where all health data can flow freely. Even when organizations want to implement interoperability solutions, the lack of cooperation or standardization among stakeholders can delay or derail efforts.
4. High Implementation Costs
The integration of interoperability into healthcare systems requires significant investment. Hospitals, medical practices, and other healthcare organizations must upgrade their IT infrastructure, train staff, and adopt new systems. Smaller healthcare providers or rural clinics may find it financially prohibitive to implement these technologies.
Additionally, the cost of implementing interoperability solutions is not limited to the initial investment. Ongoing maintenance, security updates, and the need for continuous training further increase the financial burden.
5. Resistance to Change
The healthcare industry is traditionally slow to embrace change, and many healthcare providers and administrators are resistant to adopting new technologies. This resistance is often driven by concerns about disruption, unfamiliarity with new systems, and the perceived complexity of implementing interoperability solutions.
Moreover, healthcare providers who are already using their own proprietary systems may be reluctant to switch to new solutions that enable interoperability. The cost and time required for such a transition may seem daunting, especially if they do not see immediate benefits.
Solutions for Achieving Interoperability in Healthcare
To overcome the challenges mentioned above, various solutions can be implemented. By focusing on digital health technology and collaboration, these solutions can help pave the way for achieving interoperability in healthcare.
1. Adoption of Common Data Standards
To overcome data standardization issues, healthcare organizations should adopt common data standards such as HL7 and FHIR. These standards ensure that health data is formatted and exchanged in a way that can be universally understood by different systems. Governments, healthcare organizations, and technology providers can collaborate to ensure that standards are updated regularly and that systems are designed to be compatible with these standards.
2. Cloud-Based Solutions
Cloud technology has the potential to improve interoperability by providing centralized data storage that can be accessed by different healthcare providers in real-time. Cloud-based solutions offer scalability, security, and the ability to integrate various healthcare data sources into a single platform. This would help eliminate the need for disparate, siloed systems and streamline data exchange.
Additionally, cloud platforms can support real-time data sharing and monitoring, enabling clinicians to access the most up-to-date patient information no matter where they are.
3. Blockchain for Data Security
Blockchain technology offers a promising solution for addressing the privacy and security concerns associated with interoperability. Blockchain can provide a secure, transparent, and immutable record of health data exchanges, ensuring that patient information is protected from unauthorized access and tampering.
Blockchain can also create a more secure framework for data sharing, allowing patients to have more control over who accesses their health data. The use of blockchain for interoperability can mitigate security concerns while maintaining compliance with privacy regulations.
4. Collaborative Efforts and Partnerships
Achieving interoperability requires collaboration across the healthcare ecosystem. Healthcare providers, technology developers, regulatory bodies, and patients must work together to create solutions that facilitate seamless data exchange. Partnerships between organizations, such as health networks and tech companies, are essential for developing shared platforms that enable interoperability.
Additionally, encouraging collaboration between governments and the private sector can help establish policies that promote the adoption of interoperable systems, such as incentivizing the use of common standards or offering grants for small practices to adopt digital health technologies.
5. Government Policies and Regulations
Governments play a crucial role in fostering interoperability through regulation and policy. By setting clear guidelines and encouraging the adoption of data standards, governments can accelerate the process of creating an interoperable healthcare system. For example, the U.S. government has introduced the 21st Century Cures Act, which aims to promote interoperability and reduce information blocking.
Governments can also create incentives for healthcare organizations to adopt interoperable solutions, such as offering reimbursement for providers who use certified EHRs or participate in health information exchanges.
Conclusion
Integrating interoperability into healthcare systems is a complex but necessary step toward improving the efficiency and quality of healthcare. By overcoming challenges such as data standardization, privacy concerns, and high implementation costs, the healthcare industry can unlock the full potential of digital health technology. As we continue to address these issues, collaboration among stakeholders, the adoption of cloud-based solutions, and innovative technologies like blockchain will be key to achieving seamless data exchange and improving patient outcomes.
In the end, interoperability will not only streamline healthcare processes but also lead to a more connected, efficient, and patient-centered healthcare system—one that can adapt to the demands of modern healthcare and offer better care for patients worldwide.